Learning
Collaboratives
I-VAC Learning Collaborative & Quality Improvement Project
Enhancing Patient Communication to Improve COVID-19 Vaccine Uptake
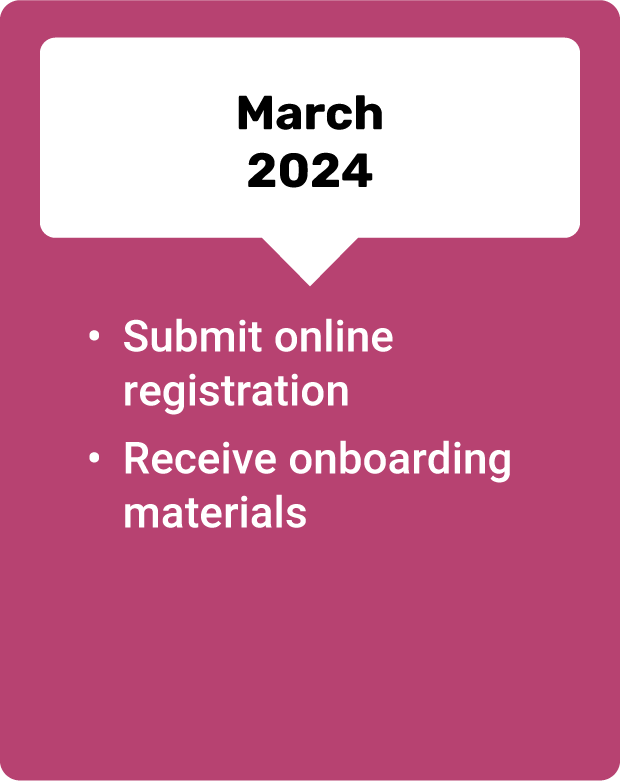
We are currently recruiting primary health care providers to join a seven-month learning collaborative and quality improvement project.

Project Goal:
To build the capacity of primary care providers to increase COVID-19 vaccination rates through improving communication with patients and families about vaccines, optimizing practice office systems, and understanding reasons for missed vaccinations opportunities during office visits.
Project Structure:
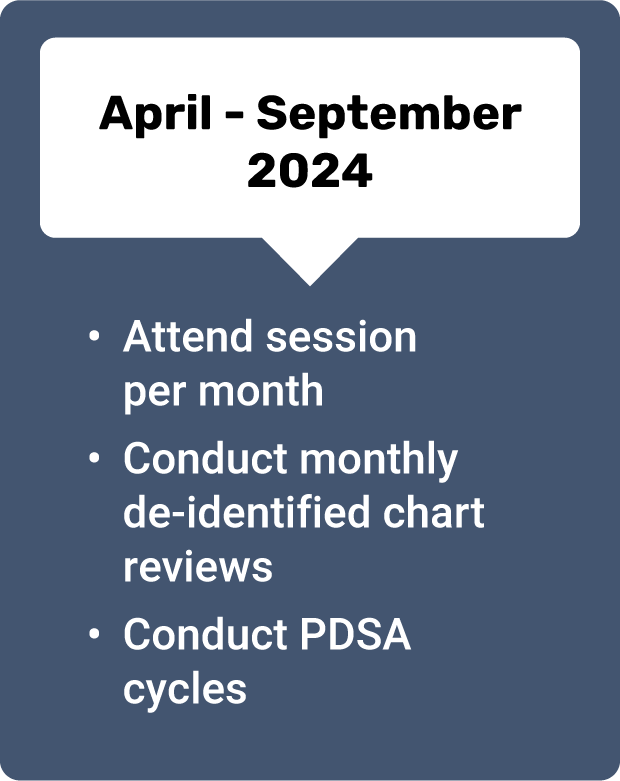
Practices will engage in monthly educational sessions that cover topics including:
- Communication techniques to overcome vaccine hesitancy
- Motivational interviewing
- Effectively using the C.A.S.E. technique
- Enhanced practice processes that promote efficient and reliable vaccine administration

Quality Improvement Project Requirements:
To participate, interested practices must:
- Provide primary care to patients in Illinois
- Complete monthly de-identified retrospective chart reviews
- Complete monthly PDSA (Plan, Do, Study, Act) cycles
Who Should Apply?
Primary care practices in Illinois who:
- Want to improve the quality of care for patients around COVID-19 vaccination and reduce vaccine hesitancy.
- Are interested in improving their practice processes around COVID-19 vaccination.
Why Participate?
This QI initiative is an easy way to earn Part 4 MOC credit and will help improve COVID-19 vaccine outreach and communication practices to drive increased vaccine uptake. Benefits include:
- Improve knowledge of best practices for office systems and care strategies to promote vaccine administration and uptake.
- Network and problem solve with others.
- Earn American Board of Pediatrics Part 4 Maintenance of Certification (MOC) credit as well as continuing medical education credits

The Illinois Chapter, American Academy of Pediatrics designates each live webinar for a maximum of 1 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. Nurses and Nurse Practitioners can submit Certificates of Attendance to their accrediting board to claim credit for participation in the live webinars.
Tackling Implementation Issues Together
Phase II of I-VAC’s implementation support is made up of a series of learning collaborative sessions open to all providers and provider organizations, regardless of participation in a Phase I COVID-19 Vaccine Bootcamp. Each learning collaborative session will focus on the practical issues of COVID-19 vaccine implementation, through a forum for providers to engage with their peers to solve the real-world barriers to implementation within their clinics and hospitals.

Focusing on the Practical
Issues of COVID-19 Vaccine
Implementation
Learning collaborative sessions focus on the practical issues of COVID-19 vaccine implementation for providers serving adult & pediatric populations, providing a forum to engage with peers and subject matter experts. Trained facilitator teams start each bi-weekly one-hour session with a very brief didactic on different best practices related to COVID-19 vaccine implementation. The remainder of the session is open for participants to share their cases or operational challenges. Following the didactic, participants will have an opportunity to share cases, stories, about the challenges that they have encountered.
Openly Discuss
Real-World Challenges
with Your Peers
Learning collaborative sessions are modeled after medical rounds, allowing participants to directly apply the knowledge they’ve gained to their own practice. Participants can openly discuss the real-world challenges of implementing recommended best practices and get advice from peers who have experienced similar situations. The learning collaboratives use the Extension for Community Health Outcomes (ECHO) model, which is a unique telementoring model based on “virtual rounding” that supports participants in translating knowledge into practice.