9. Addressing COVID-19 Vaccination Concerns for Pregnant and Nursing Mothers
Episode Description:
Santina Wheat MD, MPH, FAAFP and Corinne Kohler, MD, FAAFP talk about some of the different aspects of their experiences with patients pre-conception, during pregnancy, and while nursing. They will share conversations, additional concerns, and fears that this special population has as the decision to get vaccinated not only effects them, but it also effects the fetus and newborn. They also discuss reasons why these patients are choosing to get fully vaccinated against COVID-19 and what they can do to help protect their newborn once they go home (such as setting guidelines and communicate them to friends and family who can’t wait to meet the new baby).
The guidance for pregnant women has shifted since the COVID-19 vaccinations became available. Learn what some of these changes have been regarding the vaccine, protocols for what to do if the mother has COVID, and treatment options.
This isn’t the first time we have dealt infections in this population. Drs. Kohler and Wheat provide information to help you educate your patients who may test positive for COVID and show that we do have a track record in other infections using treatment options in the same class of medications.
Meet the Faculty
Learning Objectives:
- Understand various concerns pregnant patients have when choosing to get or not get the COVID-19 vaccine
- Identify ways to help protect the baby in utero and after delivery
Transcript:
Hello! Welcome to IVAC’s podcast series. Today we’re going to be talking about pregnancy, nursing, COVID, and COVID vaccines. I am joined today by Dr. Santina Wheat. I am Dr. Corinne Kohler, family medicine, who’s been employed at a federally qualified health center. We are going to just talk about some of the different aspects of our experiences with pregnancy, prenatal care, nursing moms, and COVID. Dr. Wheat, would you like to introduce yourself?…
Dr. Santina Wheat: Thank you so much, Dr. Kohler. So as said, I’m Dr. Tina Wheat, and I am a program director at the Northwestern McGaw Family Medicine Residency Program at Humboldt park. And I have been at Erie Family Health Centers for nine years. And I provide full scope care, including maternity care. So I think that what we’re going to talk about first is talking a little bit about why our pregnant patients are getting the COVID vaccine, and what we can talk to them about getting the vaccine.
I don’t know about you, Dr. Kohler, but I feel like when I am talking to my patients about getting the vaccine, sometimes they’re very nervous about getting it while they’re pregnant. And very worried about harming the fetus while they’re pregnant. But even the moment that they’ve delivered, they’re willing to have that vaccine. And I sometimes try to shift that conversation to talk to them about how if they get the vaccine while they’re pregnant, they’re actually doing a good job to protect their baby then and there as well. What have you seen?
Corinne Kohler, MD, FAAFP (01:37):
I would agree that that seems to be a lot of the thought processes of our prenatal women. I kind of see two groups. I see those women that come in and especially as the pandemic has progressed, are ready to get their vaccine or have gotten their vaccine. And then there’s that group that really, really either doesn’t want the vaccine or all, or wants to wait. So we spend a lot of time educating our pregnant women and their families. Our residents have done a good job at pulling some information about the antibodies. There’s now a little bit more evidence that the antibodies actually cross the placenta and protect the newborn.
A lot of times, especially if these are [inaudible 00:02:19] that we’ve seen before, we can talk about the fact that we’ve done influenza vaccine in previous pregnancies, and that has not resulted in any repercussions. Or that we use Tdap vaccine in pregnancy. So that can also open the discussions for the other vaccines. But typically if I have a woman that really doesn’t want to get the vaccine early in pregnancy, at that 36 week and weekly visit, we really are encouraging her to at least get started with the process because of how much we now know it can protect the newborn.
Dr. Santina Wheat (02:52):
I think it’s really interesting too, because I think the guidance has really shifted for pregnant women, or pregnant person. At first, we were really saying that pregnant persons would not get vaccinated. And then there was that uproar that happened because they weren’t included in the studies. And that we had just excluded a very large population.
And then I was amazed by how many, at least of my colleagues, were among the first who got the vaccine who were pregnant and physicians, and very worried about their families at home. Very worried about getting COVID because we’re in high-risk settings, and participated in the V-safe program, and so were able to add data that way. And so I don’t know about you, but I sometimes use the fact that we really used the V-safe as a way to collect additional post-study data, to have a sense of this being safe. That we’ve been able to do that in a way that I don’t think we have with other vaccines.
Corinne Kohler, MD, FAAFP (03:50):
Yeah. I agree with that. I do think that when they can see healthcare workers, especially pregnant healthcare workers, having received the vaccine, that really does encourage them. It’s one of the times to kind of use ourselves as an example. The other thing that I saw early on, about six months into the pandemic, it was actually like July of 2020. I had one of my pregnant women who was very ill in ICU. Fortunately she recovered, baby did fine, but very tight knit community.
And I will tell you within the next two months, every one of her cohort friends was in getting the vaccine. That unfortunately, while that would not have been the way I would’ve encouraged everyone to get the vaccine, once it starts rolling that way, sometimes you can use that to your benefit. But letting the women know that we consider it safe, we’re willing to get vaccinated, certainly can help promote that.
Dr. Santina Wheat (04:57):
I think it’s interesting that you talk about your patient that was sick. How have you handled when patients come to you and say, “Oh, COVID is just a cold.” And that’s why they don’t want to get this vaccine. Because they’re worried that it’s just going to be so mild, particularly when they’re pregnant?
Corinne Kohler, MD, FAAFP (05:10):
Well, and we do see some people getting COVID and having very mild symptoms. And a lot of pregnant women, we actually will end up diagnosing as positive when they come into labor and delivery. We’ve had quite a few of those that have been very low symptoms. And there seems to kind of be almost that dichotomy between the women that, while they may be more susceptible when they’re pregnant, they more often will have the mild symptoms. But then when they do get sick, they can get very sick, very quickly, and put their newborn infant or the fetus at risk.
So when people say, “This is not true.” This is not just limited to COVID. And I’ve seen this obviously with influenza vaccine over the years, as I’m sure you have also, Dr. Wheat. hat people will say, “Well, why should I get the vaccine when all I’m going to do is just be down for a day or two?” And I think the issue with COVID is, is I tell my patients, “COVID is really non-discriminatory.” It really doesn’t care if you’re young, or chronically ill, or low income, good nutrition. No matter what, it’s just kind of indiscriminate. And we don’t know who’s going to hit hard and who not. And we do know there are higher risks for obtaining COVID, but once you’ve got the COVID, we don’t know if you’re going to be in that group that’s just going to be sniffly for a couple days and may not even know they had it, or if you’re going to be one of those that’s intubated.
Dr. Santina Wheat (06:43):
Hearing that with my patients as well. And I think that what I have seen has really mirrored what some of the recent publications have said, what some of the recent data has said. Is that pregnant women are more likely to have mild symptoms, but when they do have severe symptoms, they are much more likely to be intubated or to require ICU stays. I think that most recently, the pregnant persons that I have seen that have needed that intensive care have all been infected with COVID. And it’s been something that I don’t wish on any of my patients.
Corinne Kohler, MD, FAAFP (07:14):
Right. I think that is some of the biggest challenges and hurdles we face is doing that education and putting the fetus at risk. The risk of preterm birth, the risk of stillbirth, the risk of spontaneous abortion early in pregnancy. One of the things that we don’t really know is what the long-term cognitive effects are on a newborn when the mom has been sick with COVID. And I think that’s something that … We can’t really answer that question now, but going forward, hopefully there’ll be more data that will keep coming forward as to how COVID does affect newborns going forward. What have you seen on that?
Dr. Santina Wheat (08:02):
Yeah, I haven’t seen a whole lot yet of the impacts on newborns. I’ve just been having lots of conversations about the risks that we don’t know. I tend to have these conversations when patients are asking me about the risks of the vaccine, actually. When they don’t want to get the vaccine, because they’re worried about the risks. And I will say that while we know that we have given all of these persons that have registered through the v-safe this vaccine, and we’ve been able to track these outcomes, that we also know that there’s all of these risks when they do get COVID and it seems to be much worse than any of the risks that they’re potentially worried about with the vaccine. So I think it’s a balance. Because I don’t want to do the scare tactics for my patients, I want them to be well informed and to make good decisions, but to be well aware of what their risks are.
Corinne Kohler, MD, FAAFP (08:55):
Yeah. I would agree that educating the patients and allowing them to make that choice is definitely the way I prefer to approach it. And I think one of my concerns more recently has been on some of the long COVID data coming out. I have not personally seen a lot of that in the actual pregnant population, but again, my concern is what effect that does have on the newborn. Either the newborn that where mom has gotten the COVID in utero, does that affect the newborn cognitive development, or if the newborn itself has COVID immediately after delivery? What have you told your moms about nursing and lactation if they’re COVID positive when they deliver? What has your recommendation been with that?
Dr. Santina Wheat (09:51):
We’ve asked our nursing parents to go ahead and nurse. We’ve told them to try to be cautious, and to wear a mask while they’re nursing to try to minimize the amount of time that they’re directly breathing on their baby. But at the very beginning … This was another place where it changed. At the very beginning, their newborn was isolated. But we moved away from that and are allowing the families to continue to room-in and to go ahead and breastfeed. And just to try to wear a mask while breastfeeding.
Corinne Kohler, MD, FAAFP (10:23):
Yeah. That’s been my experience also. And we generally will test the newborn. If the mom is positive in the hospital, we will test the newborn both at discharge, and then usually two to three days afterwards. Then we’ve been very fortunate in not having positive newborns coming out of the hospital. So I think continuing to nurse and pass those antibodies along, especially if they’ve been vaccinated, is something that’s definitely something to educate our moms and our families with.
Dr. Santina Wheat (10:56):
Yeah. I think we’ve had the same experience. We’ve been fortunate to not see positives come out after the positive mother in the hospital. As long as we’re talking about our pregnant persons that are testing positive for COVID, why don’t we talk a little bit about the use of treatments for COVID? And I think that there also is some hesitation around this. What are your colleagues talking about as far as COVID treatments, when patients who are pregnant test positive?
Corinne Kohler, MD, FAAFP (11:27):
I actually have not seen a lot of solid opinion on this. I think it’s varied depending on the situation and where they are in pregnancy, and such like that. But I think for the most part, the opinion now is swaying to treat early. Treat them early, treat them as soon as they’re positive. I mean, the benefits do outweigh the risk.
Again, thinking back to our days of dealing with influenza and Tamiflu for years. And initially no one wanted to use that on our pregnant ladies. And then we discovered that while it’s maybe not the most beneficial drug, the benefits do outweigh the risks, and we do use it. And I think the same thing is happening with the antivirals and the agents. Especially, I would say, second trimester, early third trimester definitely see them being used.
Dr. Santina Wheat (12:28):
So I think that it’s interesting. I recently went to a grand round where they were talking about the different therapies that were available. And I spend most of my outpatient clinical time caring for patients who are living with HIV. And one of the medications that is in the Nirmatrelvir-Ritonavir combination that goes with the brand name Paxlovid, is actually a medication that we commonly use for treating patients who are living with HIV. And have been using for patients who are pregnant and living with HIV.
And so we have fairly good data with the Ritonavir. The other medication is in the same class of medication. So I think that this is why I’ve seen our infectious disease doctors, and people like me who do both, feeling fairly comfortable with the idea of using this type of medication. Because we’ve had good experience with good pregnant person and baby out with the use of this medication.
Corinne Kohler, MD, FAAFP (13:24):
Yeah. And again, educating our patients that we do have some track record in other infections. As you said, with the HIV, what we’ve used for other viral, does kind of raise the confidence of going ahead and using them. I do see that. What other advice would you have for clinicians that are addressing pregnant women? I’m especially thinking of those family medicine docs that may do a lot of early pregnancy confirmations, maybe early prenatal, but aren’t necessarily doing daily prenatal care or doing delivery. But they have some contact with pregnant women. What kind of advice would you give those colleagues?
Dr. Santina Wheat (14:06):
I think that the advice that I want to give everybody right now, and I think pregnant patients are a special population in this too, is to not assume that the answer is going to be no for the vaccine. I was very surprised that there were some people that showed up in my office, or that I knew outside of work that had not yet gotten the vaccine. And it wasn’t because they were against it. It sometimes it was just because of convenience factor. Or they didn’t realize that they should get the booster. And so I think taking every opportunity to ask the question, and not just making an assumption that somebody is never going to get the vaccine is really important.
And just like with motivational interviewing, sometimes that first time isn’t the right time. And being able to sort of plant that seed, and see if they’ve come around after they’ve had a little bit of time to think about it. Or they’ve had so many other things on their mind that day, and now they’re in a different place to have this conversation. And never being willing to repeat the conversation … I’m sorry. Always being willing to repeat the conversation is an important piece of advice that I think we should all be following right now.
Corinne Kohler, MD, FAAFP (15:15):
Yeah, I agree. Asking every visit. And as I said earlier, we have had a cohort of women who didn’t want to get it early on, but were more willing to get it later in pregnancy. And when you don’t ask them, then of course they aren’t going to be getting it. So the advice of, everyone who’s eligible should be getting the vaccine, should really be no different.
And I find that on the rare occasion, I get a pre-conceptual counseling visit with a patient, that vaccines is definitely something that we bring up. And that was even pre-COVID, we were talk about vaccines. But especially now making sure that they go ahead and have that COVID vaccine ahead of conception, if they’re doing the pre-conceptual planning. And any of our young women of reproductive age, we really should be encouraging them to make sure they’re getting the vaccine so it doesn’t become an issue during pregnancy.
Dr. Santina Wheat (16:11):
I think that’s right. And also even if they’ve had their initial theories, reminding them, particularly if you can get that preconception visit or if you’re early on, that they’re eligible for that booster. And if anything, they’re potentially at risk more than they were before they were pregnant. And so this is really the time to make sure that they have that extra protection.
Corinne Kohler, MD, FAAFP (16:33):
So what would you say was one of the most rewarding aspects that you’ve been able to encounter with dealing with this population?
Dr. Santina Wheat (16:45):
So I love caring for my pregnant patients. I love being able to be part of their birth process. I love being able to be in all aspects of that. This might sound a little bit silly, but when I do my postpartum checks in the hospital, when I’m going around and walking through, I have a whole conversation with my patients about how their job is now to take care of themselves and to take care of their babies. And to not put anyone out for show. And having a conversation with them, but sort of giving them the power to talk to their friends and family about the rules that they want to set in their own home.
And so, I sometimes will say to them, “You can say that the doctor said. You can use me in vain. You can say that I’m the reason. ‘Nobody that’s coming around this baby shouldn’t have had a flu shot, or they need a flu shot. They need a Tdap. They need a COVID vaccine.'” Sort of giving parents the permission to put those boundaries on the people that are coming into their home. Or to say that, “Anybody that’s coming around this baby, it should wear a mask.”
And so I’ve watched sometimes the new parents have a sigh of relief that somebody else was telling them that it was okay to say this to their family members. Because sometimes their families, they’re very excited and they can be overwhelming. And so I try to give them permission. And every once in a while, just sort of seeing that change in their face or that, “Oh, I can do this,” has been a very rewarding little chunk of time that I get to spend with them in the hospital.
Corinne Kohler, MD, FAAFP (18:17):
I think that’s good advice. I generally see the women either in the office as I don’t do hospital rounds. But we do talk about the family effects. And I think COVID has given us permission even more so to say, setting the boundaries that those who come around should have their vaccines. As you said, the flu, the Tdap. Especially if they’re a caretaker, the COVID. I think that allows us to just have a little bit more freedom to say that, and a little bit more permission for the moms and the families.
I think one of the things that I really enjoy is when I get to see the whole family unit, and not just the individual pregnant women or the newborn. But when you can actually incorporate the whole family unit, and we can make sure that not just as mom needs her boundaries, but again, the family unit, the siblings, the whoever else is either close family or living in the household contacts, or will be caretakers with that that they … And that they need to be thinking not only of themselves and that infant, but bonding as a whole family.
And again, I think sometimes as we’ve looked at COVID and we see … We see this as a potentially group infection, it has actually opened those conversations to not limiting ourselves just to the women and the infant. But to be able to incorporate that, “Hey, it’s not just you. It affects those around you also.” And being able to expand that horizon.
Dr. Santina Wheat (19:58):
I think that’s a really good point. I think that’s especially true recently. I don’t know about in your area, but up here in Chicago, we’ve seen a lot of children recently actually bringing COVID home where families had been avoiding it for a while, had been doing it really well. And then the child now is bringing it home and everyone is impacted. And so it really is the entire family, as you were just saying. And that’s especially concerning when there’s someone at home that is pregnant, or there is a new baby at home.
Corinne Kohler, MD, FAAFP (20:30):
Yeah. I think we’ve seen that ebb and flow a little bit this year with our schools. And certainly after spring break, we saw a big influx in cases in the pediatric population. Hopefully that won’t continue, but I think the awareness that children can bring it home, and children can have long-term consequences, and they can share it with their siblings and their family, just helps to reinforce the concept of that we need to protect those who can’t be vaccinated. We need to protect those who can’t protect themselves.
And I think that’s part of the message to the pregnant women is, this is something for yourself, but that newborn can’t get vaccinated. There isn’t much we can do to protect the newborn in terms of vaccines, but you can help by getting vaccinated and preferably breastfeeding if able. So I think that message is one of the ones that I really, really encourage.
Dr. Santina Wheat (21:30):
Absolutely. Do you have any last thoughts Dr. Kohler?
Corinne Kohler, MD, FAAFP (21:36):
I think my last thoughts to the family medicine providers is not to shy away from asking, not to shy away from offering. As you said earlier, not to make that assumption that if they haven’t had already, that they won’t. Be willing to have that conversation. Use your motivational interviewing techniques and open it as you said, “Maybe not this time, but what are your thoughts?” But I think the biggest message I would have is just to keep the conversation open and flowing and not shy away from having that conversation with any of the family members. How about yourself?
Dr. Santina Wheat (22:16):
Yeah. I would 100% echo what you just said. And I would also really focus on specific times. So at that initial prenatal visit, maybe that’s the right time because their life is now changing and it’s an opportunity. Or when you’ve gotten past the first trimester and you’re now on the second trimester, maybe they feel a bit more comfortable. I see the postpartum visit as a really important time, because again, things have changed and they’re very focused on everything that they can do to protect themselves and they’re newborn.
And so really, not just every visit, but paying special attention to some of those big changes that are happening. And also using it this opportunity to encourage this family as well. Like I was saying, I tell people, “Anybody that’s going to be around your baby, you should have a Tdap. Everybody that’s going to be around your baby should have a COVID vaccine too.” And using it as an opportunity to spread the message for everyone.
Corinne Kohler, MD, FAAFP (23:05):
And I think encouraging the staff also. I think the staff plays a big role too, in that they can start the conversation to be part of that conversation also. It’s not limited to just the provider in the exam room. So that we set the positive atmosphere of, “This is how our clinic operates.” So any closing remarks Dr. Wheat?
Dr. Santina Wheat (23:30):
I will just say thank you so much for listening. I hope that everyone has the opportunity to encourage their pregnant patients to consider getting vaccinated. I hope that if your pregnant patients do get vaccinated, that you’ll really consider giving them the treatment to help prevent any severe disease that they might have to help prevent some of the ICU stays and needs for ventilators that we’ve seen. How about you, Dr. Kohler?
Corinne Kohler, MD, FAAFP (23:55):
I absolutely agree with how you said that. I would encourage also to avail yourself of CDC resources, the Illinois Vaccinates resources, other data and resources that are out there. If you have any questions or concerns about offering the vaccine, or what to tell your patients, or if you need any patient education material. We would very much like to thank you for joining us today. And we look forward to having you participate in further IVAC podcasts. Thank you.
Resources:
- CDC – https://www.cdc.gov/coronavirus/2019-ncov/vaccines/about-vaccines/
- Illinois Vaccinates – www.Illinoisvaccinates.com
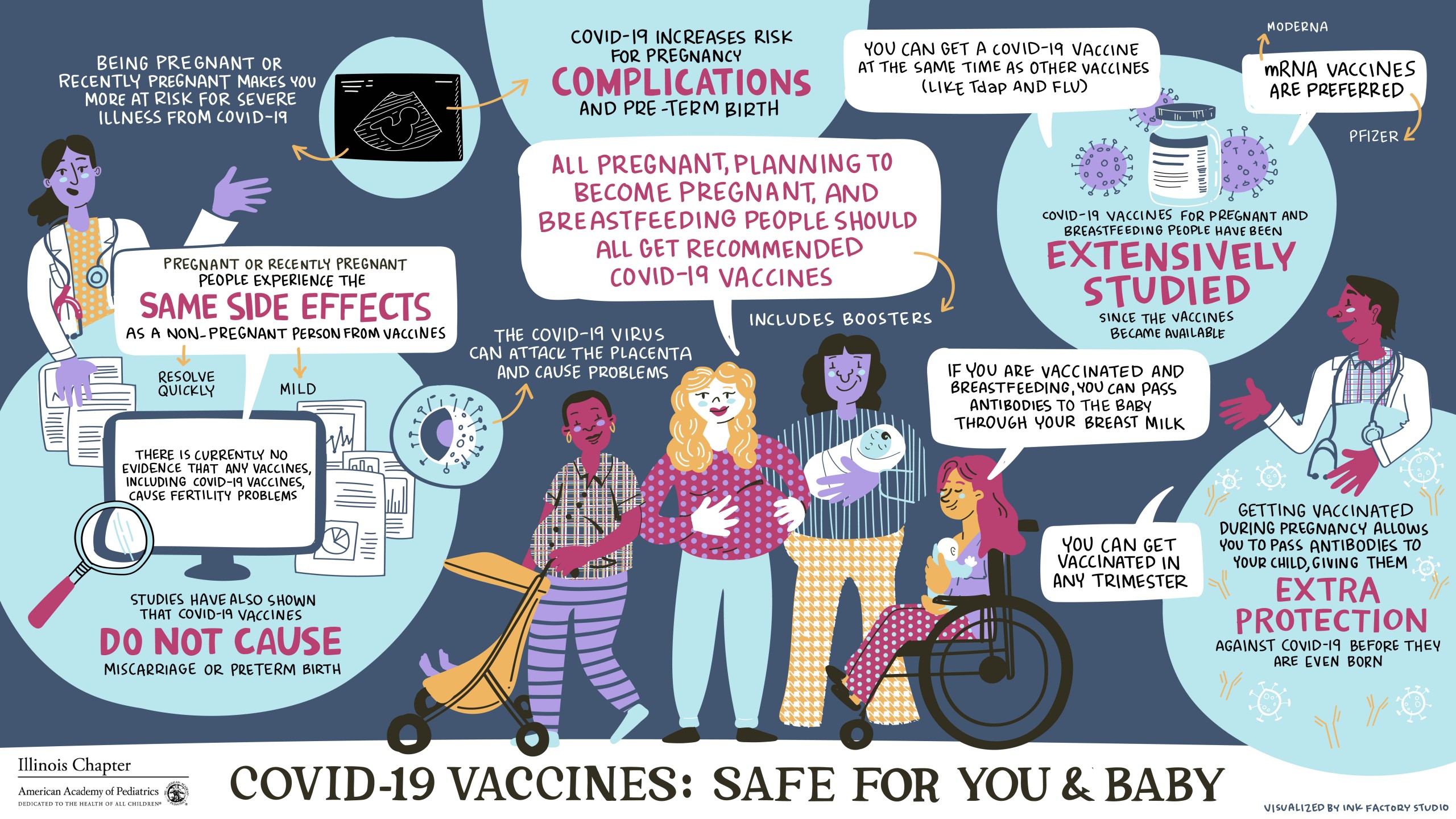
- COVID-19 Vaccines: Safe for You and Baby Poster